Tricuspid Atresia
Download this information sheet as a PDF
The aim of this information sheet is to explain what Tricuspid Atresia is, what effect it will have on a child and how it can be treated.
Animation of Tricuspid Atresia
Animation of normal heart
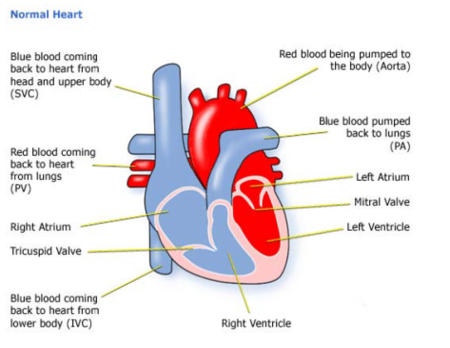
What is Tricuspid Atresia?
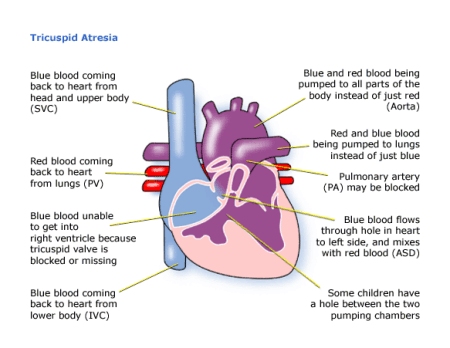
Tricuspid refers to the Tricuspid Valve.
Atresia means closed or absent.
Tricuspid Atresia results in a number of problems:
- The tricuspid valve is closed or absent
- The right ventricle is small
- The pulmonary artery is narrow
- The pulmonary valve may be blocked
The tricuspid valve should act as a gateway between the right atrium and the right ventricle, when it is missing blue (deoxygenated) blood cannot pass through the right side of the heart to the lungs.
To survive your baby will need either:
- at birth, a hole between the atria – an ASD – and a hole between the ventricles – a VSD. The ASD allows blood to cross into the left atrium, through the mitral valve and into the left ventricle. Most of it will be pumped into the aorta, but some will cross the VSD and move into the pulmonary artery (if it is not too narrowed or blocked) and so to the lungs.
- a Ductus Arteriosus. The Ductus Arteriosus is a part of our circulation before we are born, and
usually closes shortly after birth. It links the aorta to the pulmonary artery, allowing some blood to get to the lungs and can be made to remain open using drugs in the first few days of life.
Diagnosis
Tricuspid Atresia may sometimes be picked up before birth on a scan when only three chambers can be seen. If not, after birth a baby will be diagnosed early on – depending on how much blood is getting to the lungs – because he or she will look blue, have problems feeding because of breathlessness and the sound of blood moving in the wrong direction through the heart which can be heard as a heart murmur. When your baby is born how badly affected your baby is will depend on how much blood is getting to the lungs. If the pulmonary artery is narrowed (stenotic) these symptoms will be apparent very early.
- pulse, blood pressure, temperature, and number of breaths a baby takes a minute
- listening with a stethoscope for changes in the heart sounds
- an oxygen saturation monitor to see how much oxygen is getting into the blood
- a chest x-ray to see the size and position of the heart
- an ECG (electrocardiogram) to check the electrical activity
- an ultrasound scan (echocardiogram) to see how the blood moves through the heart
- checks for chemical balance in blood and urine
- a catheter or Magnetic Resonance Imaging test may be needed
Treatment
As soon as the diagnosis is made, the baby is moved to a paediatric cardiac unit, and medicine is given to keep the Ductus Arteriosus open.
The baby will need surgery when a few weeks or months old – depending on how he or she is coping. This could mean taking an artery which normally carries blood to the arm and diverting it during an operation to the pulmonary arteries so that a larger blood supply will pick up oxygen from the lungs (a Blalock-Taussig or BT shunt). This operation is done through the side of the chest while the heart is still beating.
Further surgery will need to be carried out to improve the amount of blood picking up oxygen from the lungs.
This may be:
- a Glenn / Cavopulmonary / HemiFontan Shunt – this involves making a passage between the superior vena cava (the big vein bringing blue blood from the upper body to the heart) to the right lung (pulmonary) artery. This means that a much larger amount of blue blood will flow into the lungs and pick up oxygen.
- a Fontan / Total Cavo-Pulmonary Connection. This operation joins the inferior vena cava to the pulmonary arteries as well to provide additional blood to the lung to pick up oxygen.
These are open heart surgeries – the heart will need to be stopped and opened to repair it. This means that a machine will have to take over the job that the heart and lungs normally do– the heart bypass machine.
The aim of the operations is to increase the amount of blood picking up oxygen from the lungs. The success will depend on how well the blood can flow into the pulmonary arteries from the low pressure veins.
Which of these operations is used will depend on the size of the pulmonary arteries and the pressures within them. Your child may need catheter tests to measure these pressures inside the heart.
Some children will need to continue on diuretic medicines to help them get rid of excess fluid. In some cases an anticoagulant medicine, such as aspirin or warfarin, will be prescribed. This is because blood flowing at low pressure (there is no pumping from the right ventricle) could cause a blood clot (a thrombosis).
The length of time in hospital can be several weeks and a longer period may be needed in an intensive care or high dependency unit while the heart and lungs adjust to the different pressures.
How the child is affected
After the major surgeries your child may take a long period to recover. He or she will have a scar down the middle of the chest, and there will be small scars where drain tubes were used. These fade very rapidly in most children, but they will not go altogether. Smaller scars on the hands and neck usually fade away to nothing. If the child is on warfarin, the level of anticoagulation has to be monitored frequently using a blood test (INR test – this stands for International Normalised Ratio). Some children develop a fast heart beat (a tachycardia) after surgery. This may be tackled with appropriate drugs if it is serious. Your child may develop more slowly than others and tire quickly – due to the lack of oxygen in the bloodstream. Even after the last surgery to redirect blood, he or she may not be able to catch up with others of his or her age but should be able to take part in normal activities. Most parents are amazed at how quickly their child recovers from surgery and starts to gain weight.
Some of these problems can occur after surgery or later in life:
- It is common for the valves to leak a little, but if this becomes severe, they may need further repair or even replacement with an artificial valve. If this happens the child will need to take an anticoagulant medicine to stop blood clots forming. The anticoagulant effect has to be monitored frequently using a blood test.
- A very fast heart beat (tachycardia) can happen every now and then. This may need to be corrected by drugs. If the problem continues your child may be offered an ablation (a catheter inserted through a vein can be used to stop rhythm problems occurring).
These problems may not become serious until the teen years or adulthood.
Children on Warfarin may not be able to take part in contact sports, and their INR will need monitoring. Girls should be warned against pregnancy when taking Warfarin, and should be aware that carrying a baby to term may be difficult and pregnancy may endanger their health.
Some children have other health problems and learning difficulties. It is natural to think that this is due to the surgery that the child had when he or she was very young, but they may be part of the same syndrome that caused the heart defect.
Make sure that your child is referred to a Child Development Centre so that other problems can be diagnosed as early as possible and before school-age.
Your child’s heart condition will be carefully monitored throughout his or her life.
Evidence and sources of information for this CHF information sheet can be obtained at:
(1) National Institute for Health & Care Excellence. Prophylaxis against infective endocarditis: antimicrobial prophylaxis against infective endocarditis in adults and children undergoing interventional procedures. London: NICE; 2017. Available at:
https://www.nice.org.uk/guidance/cg64
(2) Great Ormond Street Hospital. Tricuspid Valve Abnormalities Information. London: GOSH; 2017. Available at:
(3) European Journal of Cardio-Thoracic Surgery, Volume 51, Issue 6, 1 June 2017, Pages 1051–1057. Improved long-term outcomes in double-inlet left ventricle and tricuspid atresia with transposed great arteries: systemic outflow tract obstruction present at birth defines long-term outcome. Lotte C. Franken, et al. Available at:
https://doi.org/10.1093/ejcts/ezx022
About this document:
Published: May 2013
Reviewed: May 2022
To inform CHF of a comment or suggestion, please contact us via info@chfed.org.uk or Tel: 0300 561 0065.