Ventricular Septal Defect (VSD)
Download this information sheet as a PDF
The aim of this information sheet is to explain what Ventricular Septal Defect is, what effect it will have on a child and how it can be treated.
Animation of VSD
Animation of normal heart
What is Ventricular Septal Defect?
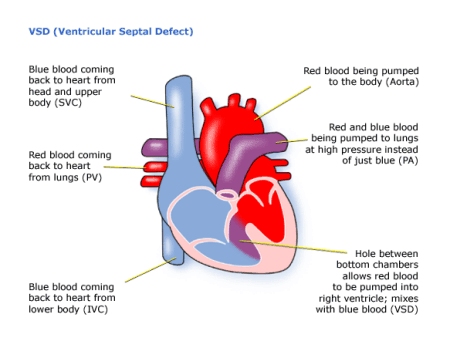
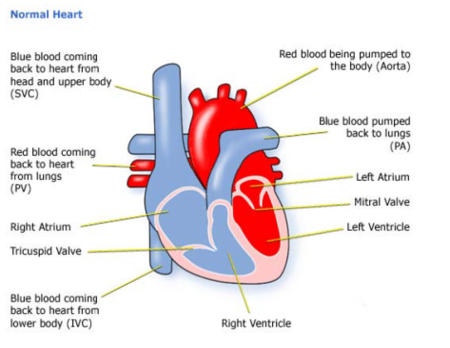
Ventricular means ‘of the ventricles’ – the pumping chambers of the heart.
Septal means ‘of the septum’ – the wall between the right and left sides of the heart.
Defect means a hole.
So a VSD is a hole in the wall between the ventricles.
Because pressure is higher on the left side of the heart, some of the blood that should be pumped into the aorta leaks from the left ventricle into the right.
A small VSD allows slightly more blood going to the lungs and does not usually require any treatment.
This kind of hole usually closes naturally or spontaneously over a period of time – sometimes not until adulthood. Small holes should not cause your child to be ill.
In a large VSD, or multiple VSD’s, the right ventricle has to work harder pumping the extra blood at high pressure into the pulmonary artery and the lungs. The left ventricle is losing blood to the right, so it has to pump harder to get enough blood into the aorta for the body’s needs. Altogether the heart and lungs have to do more work than usual.
A VSD may also occur in association with other heart defects. In some cases the VSD is necessary to allow mixing of blood in some forms of congenital heart disease such as Pulmonary Atresia.
Diagnosis
You may have had the VSD picked up in pregnancy on an ultrasound scan of the foetus.
If your baby has a large VSD, he or she may be breathless, have problems feeding, be slow putting on weight and ‘fail to thrive’. She or he may have frequent chest infections.
The sound of extra blood from a large or small VSD moving through the valve to the lungs can be heard as a heart murmur.
When a heart problem is suspected the tests used can be:
- pulse, blood pressure, temperature, and number of breaths a baby takes a minute
- listening with a stethoscope for changes in the heart sounds
- an oxygen saturation monitor to see how much oxygen is getting into the blood
- a chest x-ray to see the size and position of the heart
- an ECG (electrocardiogram) to check the electrical activity
- an ultrasound scan (echocardiogram) to see how the blood moves through the heart
- checks for chemical balance in blood and urine
- a catheter or Magnetic Resonance Imaging test may be needed.
At home
You may be at home while your baby grows with regular out-patient checks:
- You, your GP and Health Visitor should have details of your baby’s condition from the heart doctor (paediatric cardiologist). If not, call the hospital at which your baby was treated, ask for the name of the paediatric cardiologist and their telephone number. Call and explain that you need the information to pass on to, for example, your local accident and emergency department should he or she have a sudden illness.
- You should have the number of a cardiac liaison nurse or outreach nurse to call should you have questions or any fears about your baby’s heart problem.
- You should have the number of a parent support group.
Treatment
In some cases the VSD will close over time and does not need treatment – it will need to be monitored to make sure it is diminishing in size and not affecting the child’s health in any way. It is also important to ensure that there are not any other associated defects in the heart as your child grows older.
If the heart is not coping with the extra work a VSD is causing, the baby is said to be in ‘heart failure’. This can mean that the lungs and other organs become heavy with fluid (‘wet’). Your baby may then need medicines to get rid of the extra fluid – diuretics or captopril.
If the VSD is large or your baby develops ‘heart failure’ then the hole will need to be closed with an operation. Sometimes a band is placed around the pulmonary artery to reduce the blood flowing to the lungs. This is a smaller operation and allows a baby to grow and develop before the hole is closed at a further operation usually some months later.
The hole is closed using open heart surgery – the heart will need to be stopped and opened to repair it. This means that a machine will have to take over the job that the heart normally does – the heart bypass machine.
The aim of the operation is to make the circulation of blood through the heart and lungs normal, so a patch is put over the hole between the ventricles.
For most children this surgery is low risk, but it can depend on how well your child is otherwise. The doctors will discuss risks with you in detail before asking you to consent to the operation.
The length of time in hospital will usually be only a week or so, of which one or two days will be spent in the ICU depending on how well the child is otherwise.
How the child is affected
No two heart defects are the same, so there cannot be guarantees of how well your child will do. If the hole is near a valve, or there is any other problem in the heart, treatment can be more difficult, even if the VSD itself is quite small. It is not uncommon for a child to pick up an infection, such as a chest infection or infected wound, while undergoing treatment. And some children react badly to some kinds of medicines.
Most children are completely well, active, and gaining weight a few days after surgery. He or she will have a scar down the middle of the chest, and there may be small scars where drain tubes were used. These fade very rapidly in most children, but they will not go altogether. Smaller scars on the hands and neck usually fade away to nothing.
After the first year, the child will be monitored infrequently by a cardiologist.
Some of these problems can occur after surgery or later in life:
- A small amount of blood may still ‘shunt’ (or pass through the hole from the left to right sides) where the VSD is not completely closed. This should close by itself eventually.
- The aortic valve may leak because of the abnormal blood flow and may need repair at a later date.
These problems may not become serious until the teen years or adulthood.
Evidence and sources of information for this CHF information sheet can be obtained at: (1) National Institute for Health & Care Excellence. Transcatheter endovascular closure of perimembranous ventricular septal defect. Interventional procedures guidance. London: NICE; 2017. Available at:www.nice.org.uk/guidance/ipg336 (2) World Journal for Pediatric and Congenital Heart SurgeryVol 8, Issue 5, pp. 564 – 569 First Published September 13, 2017 Promoting Pulmonary Arterial Growth via Right Ventricle-to-Pulmonary Artery Connection in Children With Pulmonary Atresia, Ventricular Septal Defect, and Hypoplastic Pulmonary Arteries Edon J. Rabinowitz, MD, et al. Available at:https://doi.org/10.1177/2150135117717266 About this document: Published: May 2013Reviewed: May 2022
To inform CHF of a comment or suggestion, please contact us via info@chfed.org.uk or Tel: 0300 561 0065.










[…] was born with Ventricular Septal Defect (VSD), Transposition of the Great Arteries (TGA), Pulmonary Stenosis and various other non-heart related […]