Persistent Ductus Arteriosus (PDA)
Download this information sheet as a PDF
The aim of this information sheet is to explain what Persistent Ductus Arteriosus is, how it can affect the heart and how it is treated.
Animation of PDA
Animation of normal heart
What is Persistent Ductus Arteriosus?
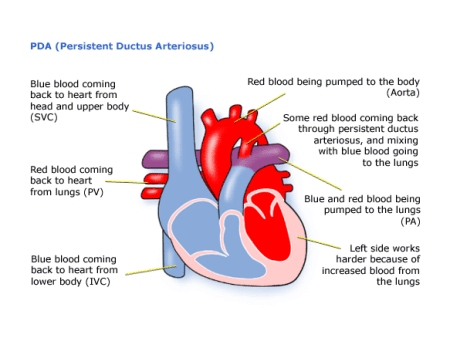
Persistent means continuing to exist. Ductus arteriosus (or arterial duct) is the name of the tube that carries blood between the aorta and the pulmonary artery in the foetus. So Persistent Ductus Arteriosus (PDA) is a tube that continues to ‘exist’ in the baby even after he or she is born.
In newborn babies, the ductus arteriosus normally closes at or shortly after birth. Sometimes, however, the mechanism of closure does not work and the connection continues to remain open – Persistent Ductus Arteriosus. This condition is also called Patent (meaning open) Ductus Arteriosus.
Before birth, the normal foetal circulation depends on the passage of blood from the pulmonary artery to the aorta through the Ductus Arteriosus. The duct starts to close in the first hours after birth. If the duct does not close, blood will pass from the aorta to the pulmonary artery and into the lungs. This will give the heart and lungs extra work to do.
This is a common condition in babies who are born prematurely. Sometimes a PDA will exist alongside other heart conditions, e.g. Aortic Stenosis. In rare cases, the cardiologist may use a medicine called Prostaglandin to deliberately keep the duct open. For example, in conditions like Pulmonary Atresia, this will increase the amount of blood going to the lungs. In conditions like Aortic Stenosis it increases the amount of blood getting into the aorta and so to the body.
Diagnosis
PDA cannot be diagnosed during pregnancy as it is part of the normal foetal circulation system. After birth your baby may be breathless, have problems feeding, or struggle to put weight on. They may also have frequent chest infections.
Many babies and children will have no symptoms, and the presence of a PDA is only noticed because of a Heart murmur. This heart murmur is the sound of blood moving through the duct and is normal in many babies in the first few days of life as the duct closes down.
When a heart murmur is heard the tests used can be:
- pulse, blood pressure, temperature, and number of breaths a baby takes a minute
- listening with a stethoscope for changes in the heart sounds
- an oxygen saturation monitor to see how much oxygen is getting into the blood
- a chest x-ray to see the size and position of the heart
- an ECG (electrocardiogram) to check the electrical activity
- an ultrasound scan (echocardiogram) to see how the blood moves through the heart
- checks for chemical balance in blood and urine
- a catheter or Magnetic Resonance Imaging test may be needed
In older children the diagnosis is usually made initially because of a heart murmur, and they may only need an echocardiogram to confirm the PDA.
Treatment
If the duct is very large, especially in premature babies, the first treatment is medical.
Medicines may be given to premature babies to try to get the ‘ductus’ to close. If these medications cannot be used, depending on the size of the Ductus Arteriosus, surgery may be needed.
In babies who are breathless or have difficulty feeding because of the extra blood going to the lungs through the Ductus Arteriosus, the lungs can become heavy or ‘wet’ with fluid. If this is the case, your baby may need medication to get rid of the extra fluid (diuretics).
Because the duct is outside of the heart, it can be closed surgically without needing to stop the heart or use a bypass machine. Surgery will involve closing-off the Ductus Arteriosus to stop blood flowing through it.
After surgery, your child will be left with a small scar on the left side of the chest. The hospital stay is often a short one of not more than a few days, depending on how well the child was before the surgery. If your child is premature then they may need to remain in hospital for a longer period of time.
Most PDAs in older infants and children are closed without surgery. A long thin tube called a catheter is used to place a closure device – usually a coil or plug – in the Ductus Arteriosus.
The catheter is threaded through a blood vessel from the groin, through the heart and into the duct, where the device is allowed to expand and block it. The hospital stay will be one or two days.
For most children the catheter procedure and the surgery are low risk, but it can depend on how well your child is otherwise. The doctors will discuss risks with you in detail before asking you to consent to the operation.
How the Child is Affected
Children should be completely well after surgery or closure by catheter, but it can depend on how well your child is otherwise. They will usually need to be monitored for about two years, and if all is well, may not need any further follow up.
Evidence and sources of information for this CHF information sheet can be obtained at:
(1) National Institute for Health & Care Excellence. Endovascular closure of patent ductus arteriosus. London: NICE; 2017. Available at:
https://www.nice.org.uk/Guidance/IPG97
(2) NHS Choices. Congenital Heart Disease Treatment. London: NHS; 2017. Available at:
http://www.nhs.uk/conditions/congenital-heart-disease/pages/treatment.aspx
(3) Insights from the Congenital Catheterization Research Collaborative. Circulation 2017. 029987. AHA. A Comparison Between Patent Ductus Arteriosus Stent and Modified Blalock-Taussig Shunt as Palliation for Infants with Ductal-Dependent Pulmonary Blood Flow. Andrew C. Glatz, et al. Available at:
http://circ.ahajournals.org/content/early/2017/10/16/CIRCULATIONAHA.117.029987.short
(4) Doppler Echocardiography in Infancy and Childhood. Patent Ductus Arteriosus. Hofbeck M., et al. (2017) Springer. Available at:
https://link.springer.com/chapter/10.1007/978-3-319-42919-9_5
About this document:
Published: June 2013
Reviewed: May 2022
To inform CHF of a comment or suggestion, please contact us via info@chfed.org.uk or Tel: 0300 561 0065.