Kawasaki Disease
Download this information sheet as a PDF
The aim of this information sheet is to explain what Kawasaki disease is, how it can affect the heart and how it is treated.
Kawasaki disease is named after Dr. Tomisaku Kawasaki, a Japanese doctor who identified the condition in 1967. Kawasaki disease causes a high fever, enlarged lymph glands and swollen blood vessels, and can also cause damage to the heart. Kawasaki disease affects more boys than girls and is usually found in children under five years of age.
How does Kawasaki disease affect the heart?
Kawasaki disease can affect the heart in the following ways:
- Coronary artery aneurysms
- Leakage of valves
- Accumulation of fluid around the heart (called pericardial effusion).
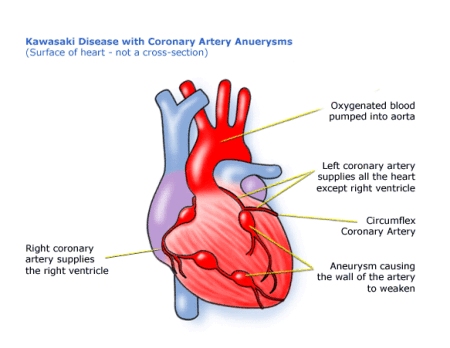
The most serious of these complications are the coronary artery aneurysms. The coronary arteries are the blood vessels that take oxygen rich blood to the heart muscle. An aneurysm is an area of a blood vessel that has become dilated and swollen.
When an artery is dilated (wider than normal), the blood flows through it more slowly because it is at a lower pressure. This change in pressure and speed makes it easier for blood clots to form which can lead to heart attacks.
In time, the coronary artery aneurysms may heal. Problems can also happen at this stage because the healed sections may be narrower than the rest of the artery (stenosis).
Kawasaki disease with coronary artery aneurysms
How is Kawasaki disease diagnosed?
There is no definite test that can be done to find out if a child has Kawasaki disease. However, there are a number of symptoms that help doctors to diagnose this disease:
- a fever that lasts more than 4/5 days
- red eyes or conjunctivitis (not sticky)
- a rash anywhere on the body
- red, cracked, dry lips
- a swollen tongue with white coating and red lumps (strawberry tongue)
- swollen neck (lymph) glands
- red swollen fingers and toes (the skin in these areas may peel at a later date)
- irritable, miserable behaviour
- painful joints.
Doctors may have to do tests to eliminate other diseases like scarlet fever that have similar symptoms to Kawasaki disease.
Other tests that may help them to diagnose Kawasaki disease include:
- measuring pulse, blood pressure, temperature, and number of breaths a child takes per minute
- listening with a stethoscope for changes in the sounds of the heart
- checking the blood for markers of inflammation
- checks for chemical balance in the blood and urine
- an ECG (electrocardiogram) to check the electrical activity of the heart
- an ultrasound scan (echocardiogram) to see how the blood moves through the heart.
The enlargement of the coronary arteries and any aneurysm that may have formed can usually be diagnosed using echocardiography. If the aneurysms heal later on (many years later) and bits of the artery become too narrow, this can be diagnosed by using stress tests or a catheter.
How is Kawasaki disease treated?
Children with Kawasaki disease are normally given an infusion of antibodies (immunoglobulin) and high doses of aspirin.
When the raised temperature and acute illness have settled, the child will be sent home on a low dose of aspirin. This will continue for about six weeks or until the cardiologist is happy that the heart has not been damaged by the disease. The child may need further doses of immunoglobulin or even some steroids if the fever does not settle.
Most children recover from Kawasaki disease without any long-term effects or damage to their heart.
Children who develop coronary artery aneurysms are treated with anticoagulant (anti-clotting) medicines such as Warfarin. Some children need other medicines, such as Nifedipine or Propranolol to reduce the work that the heart has to do. Children on these medicines may only be allowed to do a limited amount of exercise.
If a coronary artery aneurysm has healed and the artery has become too narrow, then it may need to be stretched again using a balloon catheter. If this will not work, then it might be necessary for a stent (a rigid framework) to be inserted by catheter to hold the artery open. Another option is open heart surgery, but usually a balloon catheter will work and the other methods of treatment are much less common.
How could a child be affected by Kawasaki disease?
Most children will make a full recovery from Kawasaki disease and will not need any special treatment. Children with heart complications should also make a good recovery once they have received treatment, although they may need to be monitored for some time to check there have been no further complications.
Evidence and sources of information for this CHF information sheet can be obtained at:
(1) National Institute for Health & Care Excellence. Kawasaki Syndrome.
Evidence search. London: NICE; 2017. Available at:
https://www.evidence.nhs.uk/Search?q=kawasaki+syndrome
(2) Great Ormond Street Hospital. Kawasaki Disease. London: GOSH; 2017. Available at:
http://www.gosh.nhs.uk/medical-information/kawasaki-disease
(3) Recent Topics in the Epidemiology of Kawasaki Disease. Kawasaki Disease. Uehara R. et al. (2017). Springer, Tokyo. Available at:
https://link.springer.com/chapter/10.1007/978-4-431-56039-5_14
(4) Pathophysiology of Kawasaki Disease. Kawasaki Disease. Rowley A.H., et al. (2017). Springer, Tokyo. Available at:
https://link.springer.com/chapter/10.1007/978-4-431-56039-5_6
About this document:
Published: January 2015
Reviewed: May 2022
To inform CHF of a comment or suggestion, please contact us via info@chfed.org.uk or Tel: 0300 561 0065.









