Hypoplastic Left Heart Syndrome (HLHS)
Download this information sheet as a PDF
The aim of this information sheet is to explain what Hypoplastic Left Heart Syndrome is, what effect it will have on a child and how it can be treated.
Animation of HLHS
Animation of normal heart
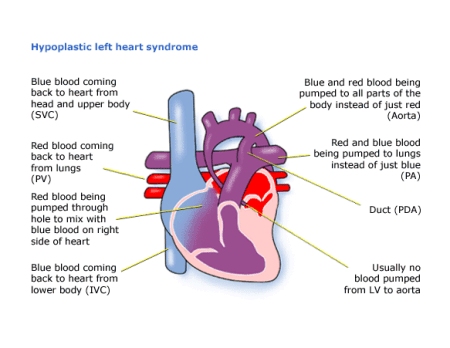
What is Hypoplastic left heart syndrome?
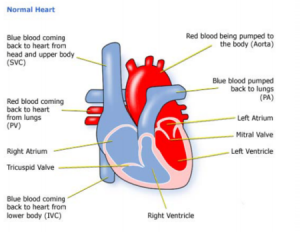
Hypoplastic means ‘not developed’. Left heart means the structures on the left side of the heart. A syndrome is a number defects together. So hypoplastic left heart syndrome (HLHS) means that the left side of the heart has not developed properly.
The left ventricle, which should pump red (oxygenated) blood to the body, is very small, and there is a virtually complete blockage between it and the aorta. The aorta, which should carry red blood to the body, is much too small.
Diagnosis
Your baby may have been diagnosed as having a heart condition before birth. HLHS may be seen on a scan of the foetal heart. HLHS can develop if there is a blocked or narrow valve, when the left side of the heart does not grow as it should during the later stages of pregnancy. Some parents decide not to continue with the pregnancy due to the difficult surgical treatment after birth.
After birth, your baby can survive while the foetal circulation system (ductus arteriosus) is still open. This is because red blood will still be crossing from the left atrium to the right. From there it will be pumped, with blue blood, into the pulmonary artery. While the ductus arteriosus is still open, blood will flow through it into the aorta, and thus round the body.
When a heart condition is detected the tests used can be:
♥ pulse, blood pressure, temperature, and number of breaths a baby takes a minute
♥ listening with a stethoscope for changes in the heart sounds
♥ an oxygen saturation monitor to see how much oxygen is getting into the blood
♥ a chest x-ray to see the size and position of the heart
♥ an ECG (electrocardiogram) to check the electrical activity an ultrasound scan (echocardiogram) to see how the blood moves through the heart
♥ checks for chemical balance in blood and urine
♥ a catheter or Magnetic Resonance Imaging test may be needed.
Treatment
HLHS is a very difficult problem to treat. The treatment for this condition is palliative. This means your child’s heart cannot be corrected, that is, made to work like a normal heart. But in some cases it can be improved with a procedure called theNorwoodoperation.
Norwood Procedure
This is a high risk procedure. It is a series of three surgical operations which would eventually allow the right side of your child’s heart to take over the work of the left side. The aim of the three operations is for the right ventricle to pump red blood to the body, while the blue blood is allowed to flow directly to the lungs.
Stage One
In the first few days of life, the wall between the left and right atrium is removed so that red blood coming back from the lungs will pass into the right atrium, and from there to the right ventricle. The pulmonary artery is detached from the lungs and made into a new aorta. A shunt (tube) is created to supply blood to the lungs either from the aorta or the right ventricle. Mixed red and blue blood will now be pumped through the new aorta to the body and to both lungs through the shunt.
Stage Two
Between the ages of four to nine months the blood flow to the lungs needs to be increased. The SVC (superior vena cava), which is a large vein carrying blue blood from the top of the body to the right atrium, is joined directly to the right lung artery. The shunt created at stage one is closed.
Stage Three
The IVC (Inferior vena cava), which is a large vein carrying blue blood from the lower part of the body to the right atrium, is also joined directly to the right pulmonary artery. This procedure is also known as the Fontan operation. This stage may be required when a child becomes more blue or breathless as more blood flow to the lungs is needed in the first few years of life or sometimes later.
There is a risk to your child in all the procedures, but how great that risk is depends on the shape of the individual heart, and how well your child is otherwise. The doctors will discuss risks with you in detail before asking you to consent to any of the operations.
Other forms of treatment
Transplantation
In some countries, some doctors recommend a heart transplant to treat HLHS in place of the 3 stageNorwoodoperation. However, transplantation is very rarely available in theUKas very few baby size hearts are offered for donation.
The surgery is palliative and does not result in a ‘cure’ so that later in life, even in adulthood, problems may develop which may result in deterioration and symptoms which are difficult to treat.
There is also a low chance of receiving a heart transplant at this stage.
How your child is affected
Treatment for HLHS is very complicated – there cannot be any guarantees of how well your child will do during or after surgeries:
You may notice some of the following things after your child’s treatment.
♥ Your child may have fluid in the lungs (pleural effusion) after surgery. It is also not uncommon for a child to pick up an infection, such as a chest infection or infected wound, while undergoing treatment. There may be other complications which your cardiologist should explain to you.
♥ Scars on the chest fade very rapidly in most children, but they will not go altogether. Smaller scars on the hands and neck usually fade away to nothing.
♥ Some children react badly to some kinds of medicines. Many children with this condition will continue to have a bluish tinge to their skin (cyanosis).
♥ Heart valves may become leaky and shunts may become too small which may require further surgery as the child gets older and bigger.
♥ The right ventricle now has to do the work of the left ventricle which it is not designed to do and may result in reduced pumping function or ‘heart failure’. This results in more breathlessness and tiredness. Medication may be used to help the heart.
♥ This unusual circulation is known to be associated with a number of long-term complications including problems with the pressure in the lung, narrowing in the lung airways and fluid in the abdomen among others.
♥ Some children develop a very fast heart rate (called tachycardia) or a slow heart rate (bradycardia). They may need medication to keep it stable, or a pacemaker to correct it.
♥ Because the flow of blood is slower than it should be, there may be a danger of blood clotting, particularly in the lungs. If the doctors think this is a concern, your child may need to take aspirin or warfarin. Aspirin and warfarin are anticoagulant medicines (stop blood cells sticking together). If your child is on warfarin, they will need to have their blood tested regularly. Read more in the Information sheet ‘Warfarin
Your child may have other health problems as well. Seek advice about claiming Disability Living Allowance (DLA) if your child needs much more care than another child of their age, or if they are having problems walking.
The very long term outcomes for children with this operation are not yet known.
More information
Evidence and sources of information for this CHF information sheet can be obtained at:
(1) National Institute for Health & Care Excellence. Hybrid procedure for interim management of hypoplastic left heart syndrome in neonates. Guidance IPG246. London: NICE; 2017. Available at:
https://www.nice.org.uk/guidance/ipg246
(2) Frontiers in Pediatrics5 (2017): 25. PMC. Web. 3 Nov. 2017.
Dewan, Sukriti et al. Model of Human Fetal Growth in Hypoplastic Left Heart Syndrome: Reduced Ventricular Growth Due to Decreased Ventricular Filling and Altered Shape. Available at:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5319967/
(4) Cardiology in the Young. Utilisation of early intervention services in young children with hypoplastic left heart syndrome. Kathleen A. Mussatto, et al.
Published online: 29 August 2017. Available at:
https://doi.org/10.1017/S104795111700169X
About this document:
Published: June 2013
Reviewed: May 2022
To inform CHF of a comment or suggestion, please contact us via info@chfed.org.uk or Tel: 0300 561 0065.










[…] Hypoplastic Left Heart Syndrome (HLHS) – Children’s Heart … – Video embedded · What is Hypoplastic left heart syndrome? Hypoplastic … So hypoplastic left heart syndrome … The surgery is palliative and does not result in a ‘cure … […]