Hypertrophic cardiomyopathy
Download this information sheet as a PDF
The aim of this information sheet is to explain what hypertrophic cardiomyopathy is, what effect it will have on a child and how it can be treated.
What is hypertrophic cardiomyopathy?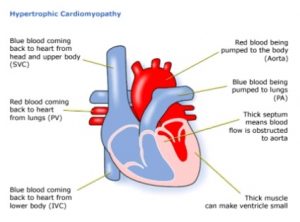
Hypertrophic means thickening. Cardio means of the heart. Myopathy is any disease of muscles. Hypertrophic cardiomyopathy (HCM) means a thickening of the heart muscle.
HCM is usually caused by a mutation (a genetic mistake). The condition can cause the heart muscle walls to thicken. This thickening occurs in the absence of any other factor or structural disorder in the heart. In some areas of the heart, the muscle cells may be found to be ‘disorganised’ (not arranged in the normal way).
SVC: Superior vena cava PV: Pulmonary valve IVC: Inferior vena cava PA: Pulmonary artery
How could HCM affect my child?
When the heart beats, it contracts to pump blood out to the body and lungs, and relaxes to fill with blood again. The function of the heart is affected by HCM.
The left ventricle (pumping chamber) does not pump enough blood. There are two reasons for this.
Firstly, the thickened muscle around it makes the ventricle smaller. This means that it does not hold as much blood as in a normal heart.
Secondly, the thickened muscle cannot relax very much so less blood is able to enter the ventricle.
- If the thickening is in the dividing wall (septum), between the left and right ventricles, it can narrow the left ventricular outflow tract (the opening to the aorta, the main blood vessel carrying blood from the heart). This reduces the amount of blood pumped out of the heart.
- The thickened heart muscle may affect the function of the heart valves. In particular, the mitral valve may become ‘leaky’ if it cannot close properly.
- The condition may cause the heart beat to become fast or erratic. This is known as arrhythmia.
HCM affects approximately 1 in 500 of the population.
Most cases of hypertrophic cardiomyopathy are caused by mutations (mistakes) in the genes. Children are not usually affected by symptoms until they are teenagers, but some do have symptoms when they are still young. It has been estimated that children only account for about 10% of HCM cases. Most cases are hereditary so screening seems to be recommended for only close, first degree relatives.
Not everyone with HCM will have any symptoms. Symptoms may develop at any stage in life and do not reflect the severity of the condition.
Possible symptoms include:
- breathlessness (shortness of breath), usually during exercise
- chest pain: the reason for pain is not clear but it may be due to not enough blood and oxygen getting to the thickened heart muscle
- palpitations: may be caused by abnormalities of the heart rhythm. This can be a fast heart beat, or skipped beats
- dizziness and fainting attacks: these can happen because of the smaller than normal quantity of blood being pumped by the heart or because of an arrhythmia (fast heart beat). Any unexplained fainting should be investigated immediately.
- HCM can cause sudden death in a small number of people affected; however, the risk of this is very small if the condition is diagnosed, monitored and treated.
How is HCM diagnosed?
HCM may be suspected in your child because a relative has been diagnosed with the condition. HCM may occur together with other genetic conditions such as Noonan syndrome or mitochondrial disorders. Sometimes HCM is a congenital problem, meaning that it emerges during the development of the foetus, but the cause may not be clear. Once the condition has been diagnosed, doctors will investigate further to identify if there is an underlying cause.
When a heart problem is suspected the tests used can be:
- pulse, blood pressure, temperature and number of breaths a child takes a minute
- listening with a stethoscope for changes in the heart sounds
- an oxygen saturation monitor to see how much oxygen is getting into the blood
- a chest x-ray to see the size and position of the heart
- an ECG (electrocardiogram) to check the electrical activity of the heart
- an ultrasound scan (echocardiogram) to see the structure of the heart and how the blood moves through the heart
- checks for chemical balance in blood and urine
- 24 hour heart monitoring to look for any abnormal heart rhythms
- an MRI scan to show the structure and function of the heart and look more closely at the pattern of the thickening
- an exercise test to see how the heart and blood pressure respond to exercise
- occasionally a catheter test is needed to look at the changes inside the heart, to measure the pressures in the heart chambers, and to check the electrical activity that regulates heartbeat.
How is HCM monitored?
HCM is a very variable condition. Some people have mild symptoms, others have severe symptoms. Sometimes the symptoms are progressive, but often once the thickening stops, it remains quite stable. Regardless of symptoms, they will need regular monitoring. This will include ECGs, echocardiograms and 24 hour monitoring. The frequency and tests needed depend upon the symptoms your child has and the findings of previous tests.
Contact the cardiologist if your child experiences any of the following symptoms:
- increased breathlessness that is interfering with their normal activities
- light-headedness
- chest pain
- fainting
How is HCM treated?
HCM can be improved and controlled by treatment including:
- drugs to control abnormal heart rhythms and relax the heart, allowing it to fill more easily
- implanting a defibrillator, if there is a risk of sudden death due to abnormal heart rhythms
- in a small number of patients, surgery may be necessary. Surgery may involve removing part of the septum that is blocking the outflow tract. If surgery is required your child’s cardiologist will discuss it with you in detail.
Evidence and sources of information for this CHF information sheet can be obtained at:
(1) National Institute for Health and Care Excellence. Implantable cardioverter defibrillators and cardiac resynchronisation therapy for arrhythmias and heart failure. Guidance TA314. London: NICE; 2017. Available at:
https://www.nice.org.uk/guidance/ta314
(2) Cardiomyopathy UK. Cardiomyopathy UK booklet: ‘Living with cardiomyopathy’. London: Cardiomyopathy UK; 2017. Available at:
(3) British Heart Foundation. Hypertrophic cardiomyopathy. London: BHF; 2017. Available at:
https://www.bhf.org.uk/heart-health/conditions/cardiomyopathy/hypertrophic-cardiomyopathy
About this document:
Published: June 2015
Reviewed: May 2022
To inform CHF of a comment or suggestion, please contact us via info@chfed.org.uk or Tel: 0300 561 0065.









